Our first product – InfectiClear®.
A precision diagnostic test.
Our AI-based blood test investigates the patient – rather than the pathogen – allowing us to rule out infection or sepsis.
We have developed a patented set of assays using advanced machine-learning techniques to diagnose infection. Trained from blood samples collected over 15 years, these samples included thousands of patients, some of whom developed infections and sepsis. The samples were collected daily and include full clinical metadata, and they have been robustly adjudicated for true clinical disease status.
Diagnostics trained & validated using a
wealth of clinical data








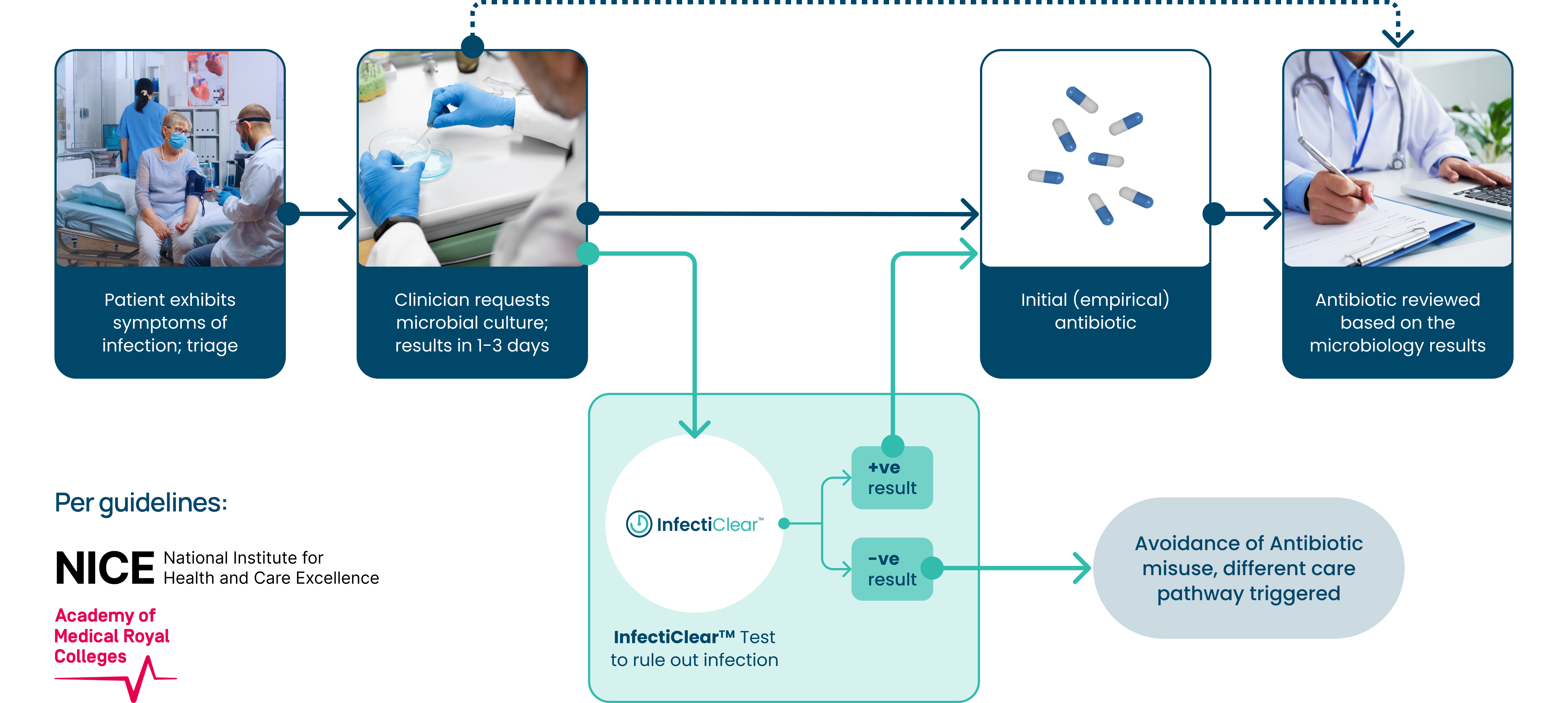
How our diagnostic tests work in practice
InfectiClear® is scheduled for release in 2025; the kit (reagents) will be available with a user-friendly, local software package. The software generates a score indicating the likelihood of infection.
This will provide clinicians with the confidence to withhold, delay, or reduce antibiotics in the event of a low-risk score.
Ease of broad deployment:
Results within care pathway
Guidelines mandate 1-6 hour investigation
Our Development

We are innovating solutions for early infection and sepsis diagnosis with a breakthrough approach that leverages 15 years of clinical research. This wealth of data will enable us to continue to ideate on our product line, reducing time to result, cost of result, and creating more opportunity for diagnostic outcomes.

We identified specific genes and biomarkers that were expressed differently between patients with infection, sepsis and other non-infectious conditions. We did this by applying proprietary machine learning and AI to our wealth of clinical data, leading to assays that can reliably predict the onset of infection and sepsis prior to clinical presentation and diagnosis.
Our Collaborators
Fueling Progress:
Our Investors and Tech Collaborators
Offering expertise and resources, our investors and tech collaborators are critical in the evolution of Presymptom Health.